Evaluation of Medication Adherence in COPD Patients and their Drug Utilization Pattern
Faheemuddin MD, Ramaiah B, Kiran SS, Kumari BS, Vijayalaxmi M
DOI10.21767/2572-5548.100017
Faheemuddin MD*, Ramaiah B, Kiran SS, Kumari BS and Vijayalaxmi M
Department of Pharmacy Practice, Smt. Sarojini Ramulamma College of Pharmacy, Mahabubnagar, Telangana, India
- *Corresponding Author:
- Faheemuddin MD
Department of Pharmacy Practice
Smt. Sarojini Ramulamma College of Pharmacy
Mahabubnagar, Telangana, India
Tel: +91-8464984963
E-mail: faheemuddin.md4u@gmail.com
Received Date: September 01, 2016; Accepted Date: October 25, 2016; Published Date: October 31, 2016
Citation: Faheemuddin MD, Ramaiah B, Kiran SS, Kumari BS, Vijayalaxmi M (2016) Evaluation of Medication Adherence in COPD Patients and their Drug Utilization Pattern. Chron Obstruct Pulmon Dis 1:17. doi: 10.21767/2572-5548.100017
Copyright: © 2016 Faheemuddin MD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Chronic obstructive pulmonary disease (COPD) is a chronic disease of longer duration and generally progressive in nature. COPD needs treatment throughout the life.
The main objective of the study is to determine whether pharmacist intervention improves the medication adherence in COPD patients. Participants were enrolled after providing and giving informed consent form.
Methodology: A prospective interventional study was conducted at the SVS a tertiary care hospital and government hospital in Mahabubnagar after getting the ethical committee permission.
Case note prescriptions were collected to observe the drugs used and an 8 item questionnaire was prepared and according to questions score was by using the Morisky medication adherence scale (MMAS). The questionnaires were used to know the medication adherence to treatment.
Results: A total of 60 patients were enrolled, out of which 35 were taken as control group who were not given any counseling and other 35 were taken as Intervention group who were given the counseling. The Morisky Medication Adherence showed the Value which was found to be highly significant i.e., <0.0001***.
Conclusion: The present study was undertaken to assess the knowledge of the patient about the disease and their adherence to therapy.
The main aim of the study is to assess medication adherence to treatment and the drug utilization pattern in COPD patients. Thus in this study the clinical pharmacist intervention brought an impact on adherence to therapy.
Keywords
COPD; Medication adherence; MMAS
Introduction
Definition
The National Heart, Lung, and Blood Institute/World Health Organization (NHLBI/WHO) Global initiative for COPD (GOLD) definition of COPD is a disease state characterized by air flow limitation that is not fully reversible. The air flow limitation is usually both progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases [1].
Chronic bronchitis: Is a common condition defined clinically as persistent cough with expectoration due to excessive mucous secretion by the tracheobronchial tree, which results in air way obstruction as a result of edema and bronchial inflammation [2].
Emphysema: The WHO defined pulmonary emphysema as combination of permanent dilation of air spaces distal to the terminal bronchioles and destruction of the walls of dilated air spaces. There is lack of uniformity in air space enlargement, resulting in loss of alveolar surface area that leads to air flow limitation. Emphysema is defined morphologically, while chronic bronchitis is defined clinically [1] (Table 1).
| Bronchitis | Emphysema |
|---|---|
| • Persistent cough is the hallmark of bronchitis; it occurs first in winter then progress to year round. It is usually worse in the morning. • Dyspnoea is generally not prominent at rest but is more on exertion. • Patients are called blue blotters due to cyanosis and edema. • Right heart failure (Corpulmonale) is common. • Bronchioles may contain mucus plugs and purulent exudates. • Other common findings include rhonchi and wheezes on auscultation, prolonged expiration and normal respiratory rate. |
• Cough is chronic but less productive than in chronic bronchitis and cough occurs late after dyspnea. • Dyspnea is progressive, constant, severe and more characteristic of emphysema than chronic bronchitis. • Patients are called pink puffers as they remain well oxygenated and have tachypnea. • Corpulmonale and hypercapneic respiratory failure are the usual terminal events. • Other findings include tachypnea, weight loss, pursed lip breathing, prolonged expiration and diminished breath sounds. |
Table 1: Clinical manifestations [2].
Aetiology
The most important etiologic factors are:
• Smoking: It is the primary factor for the development of COPD. Present in >90% of patients it impairs ciliary movement, inhibit the function of alveolar macrophages and it leads to hypertrophy and hyperplasia of mucus secreting glands. It stimulates the vagus nerve and causes bronchoconstriction.
• Atmospheric pollution: Incidence of COPD is higher in industrialized urban areas where air is polluted. Some of the atmospheric pollutants that increase risk of developing COPD are sulfur dioxide, nitrogen dioxide, particular dust and toxic fumes.
• Occupation: Workers engaged in certain occupations like cotton mills, plastic factories etc. are exposed to various organic and inorganic dusts which contribute to disabling chronic bronchitis in such individuals.
• Infection: Bacterial, viral and mycoplasmal infections do not initiate chronic bronchitis but usually occurs secondarily to bronchitis.
• Familial and genetic factors: These appear to be poor tendency to develop bronchitis [2].
• There is an increased risk of emphysema in people who are having α1- antitrypsin (ATT) deficiency. The major physiologic function of ATT is inhibition of neutrophil elastase in emphysema [1].
Pharmacological treatment
• Bronchodilators: Are used to control symptoms; no single pharmacological class has been proven to provide superior benefit over others, although inhaled therapy is generally preferred. β2 sympathomimetics cause relaxation of bronchial smooth muscle and broncho dilation by stimulating the enzyme adenylcyclase to increase the formation of cyclic adenosine monophosphate. They may improve mucociliary clearance [3].
• Anticholinergic agents: These agents produce bronchodilator by competitively inhibiting cholinergic receptors in bronchial smooth muscle. This activity blocks acetylcholine, with the net effect of being a reduction in cyclic guanosine monophosphate, which normally acts to constrict bronchial smooth muscle [4].
• Methylxanthines: These compounds typically are added to the drug regimen after an unsuccessful trail of ipratropium bromide and beta adrenergics [3].
• Corticosteroids: Exert their beneficial through reduction in capillary permeability to decrease mucus by inhibition of release of proteolytic enzymes from leukocytes and inhibition of prostaglandins.
• Antibiotics: Are used to treat exacerbations with suspected infection as evidence by increasing the volume or change in the color or viscosity of sputum, along with dyspnea.
• Mucolytics: (oral n-acetylcysteine) may improve the sputum clearance and disrupt mucous plugs.
• Expectorants: (e.g. guaifenesin) may be used. Potassium iodide should be avoided because of side effects associated with the iodine therapy.
• Antioxidants: (e.g. oral n-acetylcysteine) may reduce exacerbations frequency [5].
Role of medication adherence in COPD
Medication adherence is defined as the extent to which a patient’s medication taking behavior coincides with the intention of the health advice he/she has been given. Adherence is one of the most important factors that determine therapeutic outcome, especially in patients suffering from chronic illness like COPD. Adherence is nothing but a medication taking behavior. It is extremely important for better therapeutic outcome in many situations like replacement therapy, maintenance of pharmacological effect, maintenance of serum drug concentrations to control [6].
Non adherence to medication can occur in situations like forgetfulness, poor communication, lack of motivation, emotional concern, family dynamics, financial constraints, inadequate health literacy, poor patient knowledge, belief about the illness, and its severity, cause, prevention and treatment. These barriers can be overcome through effective counseling by the pharmacist. Pharmacists are in a unique position to improve medication adherence because they can actually show the medication to the patient and provide any information related to the medication [7].
Drug utilization evaluation (DUE)
Drug utilization evaluation/review are defined by WHO as marketing, distribution, prescription and use of drugs in a society with special emphasis on the resulting medical, social and economic consequences.
The 3 types of DUE are Prospective, Concurrent and Retrospective. A retrospective DUE is performed after the patient has received the medication / drug therapy. It may detect patterns in prescribing, dispensing or administering drugs to prevent recurrence of inappropriate use or abuse, and serves as a means for developing prospective standards and target intervention. Patient medical charts or computerized records are screened to determine whether the drug therapy met approved criteria and aids prescribers in improving care for their patients, individually and group-wise [8].
Materials and Methods
This is a prospective interventional study carried out in pulmonary department of SVS medical college hospital and government hospital, Mahabubnagar where patients eligible according to the inclusion criteria are enrolled in to the study after obtaining the consent. The data collection form will be prepared and used. This form mainly contains the demographic details of the patient, medication chart, MMAS-8 scale and Patient information leaf lets.
All information relevant to the study will be collected at the time of admission to till the date of discharge and the data will be analyzed using suitable statistical method.
Results
A study was carried out at Mahabubnagar in which 60 patients were enrolled. Out of 60, 30 were given taken as intervention group and other 30 were taken as control group. The results of the study are as follows:
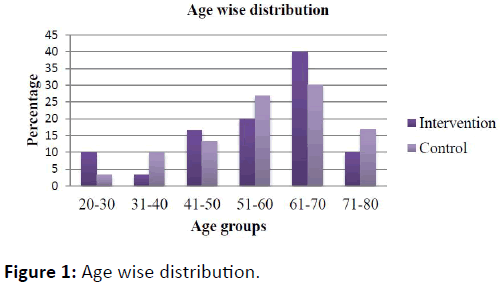
It shows that in the age group of 61-80 i.e., (40%) of the patients are high in number and less number of people was found in the age group of 21-40 i.e., (2.8%) (Figure 1).
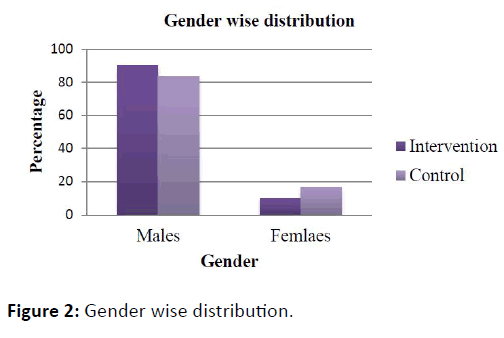
In gender wise distribution there are more number of males both in intervention group and control group patients in comparison to females (Figure 2).
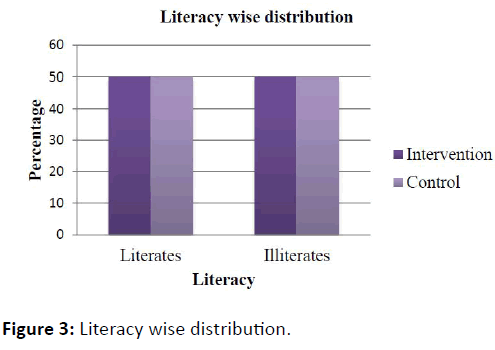
In the literacy wise distribution there is an equal number of the patients were found in both intervention and the control group (Figure 3).
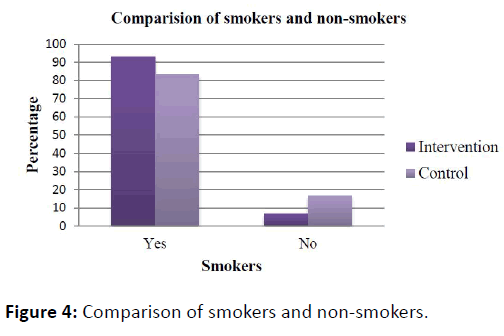
In smokers and non-smoker’s comparison, there is high percentage of smokers in both intervention group and control group and less percentage of non-smokers (6.7%) in the intervention group (Figure 4).
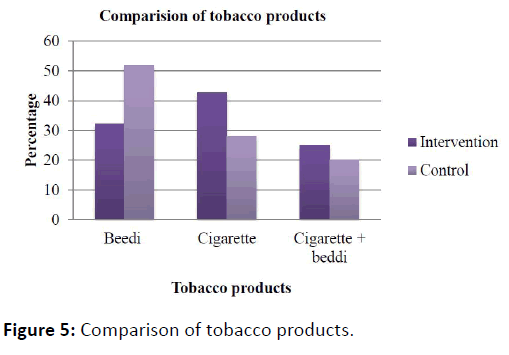
The tobacco products usage in the intervention group were using more number i.e., cigarette followed by beedi and then cigarette + beedi in combination when compared the control group (Figure 5).
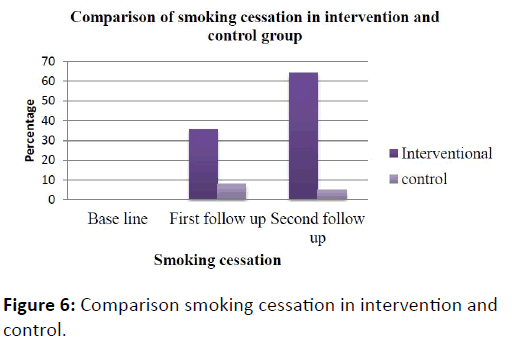
In the interventional group there were 28 members smokers at the base line and for first follow-up 10 (35.7%) members stopped smoking and for the second follow up 18 members stopped smoking and in the control group at baseline 25 members were smokers at the baseline and 2 (8%) members stopped smoking at the first follow-up and 5 (20%) members stopped at the second follow-up (Figure 6).
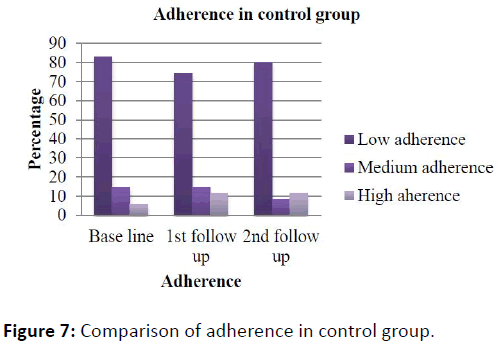
In 30 control patients were of low adherence in base line and there was a same adherence in the patient after the two followups (Figure 7).
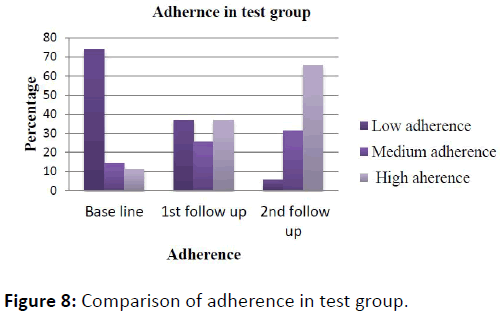
In the interventional group there was a low adherence in base line and there was an improved adherence after counseling and follow up of patients (Figure 8).
Morisky medication adherence scale scores
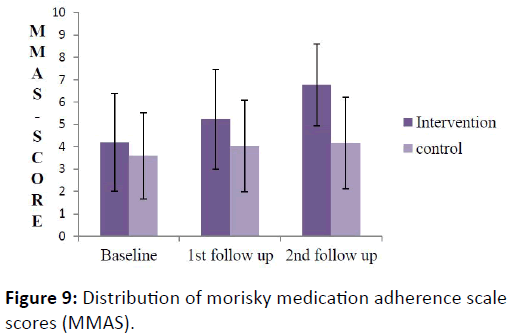
In this study total 60 patients were enrolled out of 60, 30 were taken as the control group and the other 30 were taken as intervention group. The p values at the base line medication adherence was no difference, followed by first follow up was <0.01* followed by second follow up was <0.0001*** (Figure 9, Table 2).
| MMAS | Intervention group | Control group | P value |
|---|---|---|---|
| Baseline | 4.2 ± 2.19 | 3.6 ± 1.94 | ns |
| 1st follow up | 5.2 ± 2.22 | 4.03 ± 2.06 | P<0.01* |
| 2nd follow up | 6.8 ± 1.83 | 4.17 ± 2.05 | P<0.0001*** |
Table 2: Distribution of morisky medication adherence scale scores (MMAS).
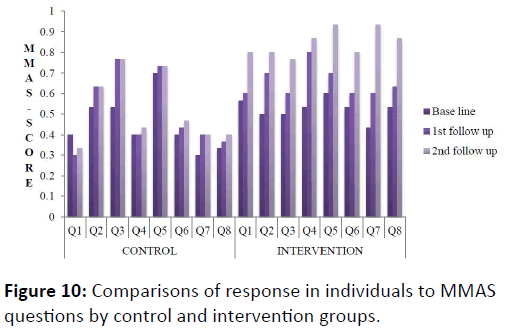
The response in the individuals of the intervention and control group to the individual questions in the MMAS-8 questionnaire (Figure 10, Table 3).
| MMAS | Control(N=30 ) | Intervention (N=30) | |||||||||
| Correct Response | % | Mean | std | Correct Response | % | Mean | Std | P value | |||
| 1.Do you sometimes forget to take yourmedicine | |||||||||||
| Base line | 12 | 40 | 0.4 | 0.50 | 17 | 56.6 | 0.57 | 0.5 | |||
| 1stfollow up | 9 | 30 | 0.3 | 0.47 | 18 | 60 | 0.6 | 0.5 | 0.7122 | ||
| 2nd follow up | 10 | 33.33 | 0.33 | 0.48 | 24 | 80 | 0.8 | 0.41 | 0.0169* | ||
| 2.People sometimes miss taking their medicines for reasons other than forgetting. Thinking over the past 2weeks, were there any days when you did not take your medicine? | |||||||||||
| Base line | 16 | 53.33 | 0.53 | 0.51 | 15 | 50 | 0.5 | 0.51 | |||
| 1stfollow up | 19 | 63.33 | 0.63 | 0.49 | 21 | 70 | 0.7 | 0.47 | 0.0117* | ||
| 2nd follow up | 19 | 63.33 | 0.63 | 0.49 | 24 | 80 | 0.8 | 0.41 | 0.0014** | ||
| 3.Have you ever cut back or stopped taking your medicine without telling your doctor because you felt worse when you took it? | |||||||||||
| Base line | 16 | 53.33 | 0.53 | 0.51 | 15 | 50 | 0.5 | 0.51 | |||
| 1st follow up | 23 | 76.67 | 0.77 | 0.43 | 18 | 60 | 0.6 | 0.5 | 0.1841 | ||
| 2ndfollow up | 23 | 76.67 | 0.77 | 0.43 | 23 | 76.67 | 0.77 | 0.43 | 0.0089** | ||
| 4.When you travel back or leave home, do you sometimes forget to bring along your medicine? | |||||||||||
| Base line | 12 | 40 | 0.4 | 0.5 | 16 | 53.33 | 0.53 | 0.51 | |||
| 1stfollow up | 12 | 40 | 0.4 | 0.5 | 24 | 80 | 0.8 | 0.41 | 0.0089** | ||
| 2ndfollow up | 13 | 43.33 | 0.43 | 0.5 | 26 | 86.67 | 0.87 | 0.35 | 0.0054** | ||
| 5.Did you forget to take all your medicines yesterday? | |||||||||||
| Base line | 21 | 70 | 0.7 | 0.47 | 18 | 60 | 0.6 | 0.5 | |||
| 1stfollow up | 22 | 73.33 | 0.73 | 0.45 | 21 | 70 | 0.7 | 0.47 | 0.1841 | ||
| 2ndfollow up | 22 | 73.33 | 0.73 | 0.45 | 28 | 93.33 | 0.93 | 0.25 | 0.0007*** | ||
| 6.When you feel like your symptoms are under control, do you sometimes stop taking your medicine? | |||||||||||
| Base line | 12 | 40 | 0.4 | 0.5 | 16 | 53.33 | 0.53 | 0.51 | |||
| 1stfollow up | 13 | 43.33 | 0.43 | 0.5 | 18 | 60 | 0.6 | 0.5 | 0.4888 | ||
| 2nd follow | 14 | 46.67 | 0.47 | 0.51 | 24 | 80 | 0.8 | 0.41 | 0.0029** | ||
| 7. Taking medicine every day is a real inconvenience for some people. Do you ever feel hassled about sticking to your treatment plan? | |||||||||||
| Base line | 9 | 30 | 0.3 | 0.47 | 13 | 43.33 | 0.43 | 0.50 | |||
| 1stfollow up | 12 | 40 | 0.4 | 0.50 | 18 | 60 | 0.60 | 0.50 | 0.096 | ||
| 2nd follow | 12 | 40 | 0.4 | 0.50 | 28 | 93.33 | 0.93 | 0.25 | P<0.0001*** | ||
| 8. How often do you have difficulty remembering to take all your medicine? A. Never/ rarely B. Once in a while C. Sometimes D. Usually E. All the time |
|||||||||||
| Base line | 10 | 33.33 | 0.33 | 0.48 | 16 | 53.33 | 053 | 0.51 | |||
| 1stfollow up | 11 | 36.67 | 0.37 | 0.49 | 19 | 63.33 | 0.63 | 0.49 | 0.2638 | ||
| 2nd follow | 12 | 40 | 0.40 | 0.50 | 26 | 86.67 | 0.87 | 0.35 | 0.0023** | ||
Table 3: Comparisons of response in individuals to MMAS questions by control and intervention groups.
Drug utilization pattern
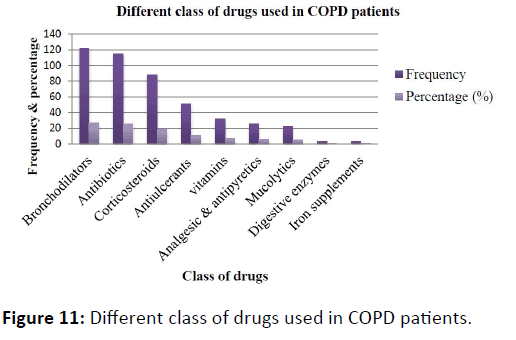
Different class of drugs used in COPD patients: A total number of 461 drugs of different class were prescribed in the prescription of 60 COPD patients. An average of 7-8 drugs was prescribed in each prescription (Figure 11, Table 4).
| Class of drugs | Frequency | Percentage (%) |
|---|---|---|
| Bronchodilators | 122 | 26.4 |
| Antibiotics | 115 | 24.9 |
| Corticosteroids | 88 | 19.1 |
| Antiulcerants and antisecretory | 51 | 11.1 |
| Vitamins | 32 | 6.9 |
| Analgesic & antipyretics | 25 | 5.4 |
| Mucolytics | 22 | 4.8 |
| Digestive enzymes | 3 | 0.7 |
| Iron supplements | 3 | 0.7 |
Table 4: Different class of drugs used in COPD patients.
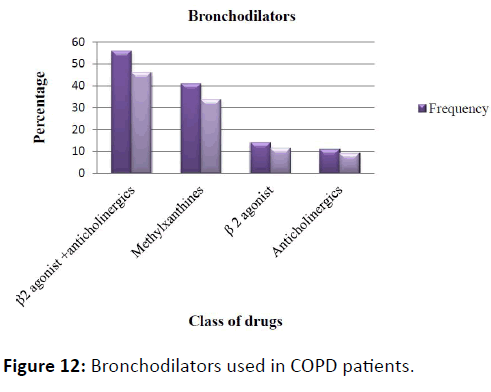
Bronchodilators used in COPD patients: The most commonly used bronchodilators in COPD patients is the combination of β2 agonist + anti-cholinergic (Salbutamol + Ipratropium bromide) (Figure 12, Table 5).
| Bronchodilators | Frequency | Percentage (%) |
|---|---|---|
| β2agonist + anticholinergic | 56 | 46 |
| Methylxanthines | 41 | 33.6 |
| β2agonist | 14 | 11.4 |
| Anticholinergic | 11 | 9 |
Table 5: Bronchodilators used in COPD patient.
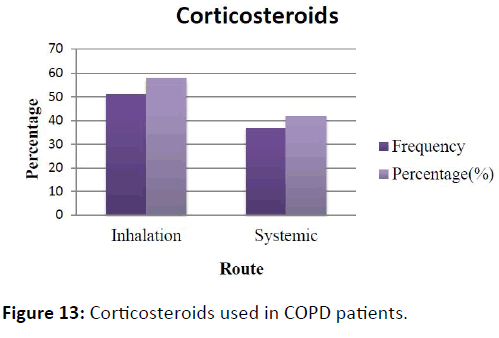
Corticosteroids used in COPD patients: It inferred that out of 60 COPD patients 88 corticosteroids were prescribed in the prescription in which systemic corticosteroids were (42%) and inhaler corticosteroids (58%) were used more than the systemic corticosteroids (Figure 13, Table 6).
| Corticosteroids | Frequency | Percentage (%) |
|---|---|---|
| Inhalational | 51 | 58 |
| Systemic | 37 | 42 |
Table 6: Corticosteroids used in COPD patients.
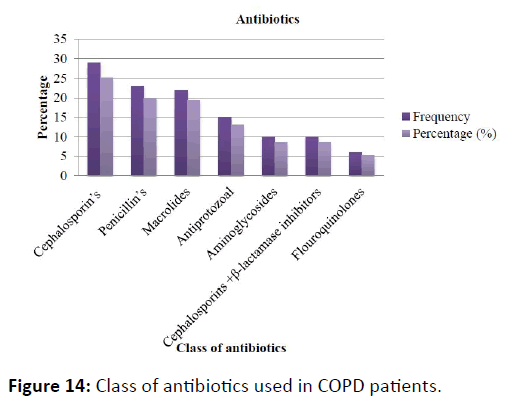
Class of antibiotics used in COPD patients: It is observed that in 60 patients different class of antibiotics were used among them cephalosporin antibiotics were used in high number than other class of antibiotics (Figure 14, Table 7).
| Antibiotics | Frequency | Percentage (%) |
|---|---|---|
| Cephalosporin’s | 29 | 25.2 |
| Penicillin’s | 23 | 20 |
| Macrolides | 22 | 19.3 |
| Antiprotozoal | 15 | 13 |
| Aminoglycosides | 10 | 8.6 |
| Cephalosporins + β-lactamase inhibitors | 10 | 8.6 |
| Flouroquinolones | 6 | 5.2 |
Table 7: Class of antibiotics used in COPD patients.
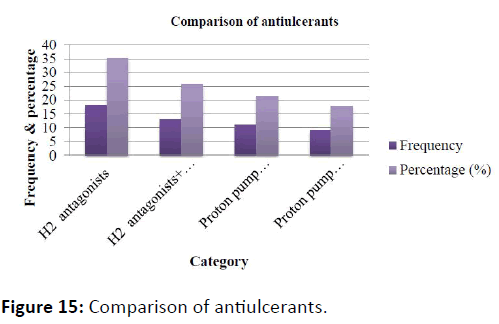
Comparison of antiulcerants: It inferred that out of 60 patients high percent of H2 receptor antagonists (ranitidine) were used and the less percent of Proton pump inhibitors + antiemetic (Rabeprazole + domperidone) were used as antiulcerants (Figure 15, Table 8).
| Category | Frequency | Percentage (%) |
|---|---|---|
| H2antagonists | 18 | 35.2 |
| H2antagonists+ antiemetic | 13 | 25.6 |
| Proton pump inhibitors | 11 | 21.5 |
| Proton pump inhibitors + antiemetic | 9 | 17.7 |
Table 8: Comparison of antiulcerants.
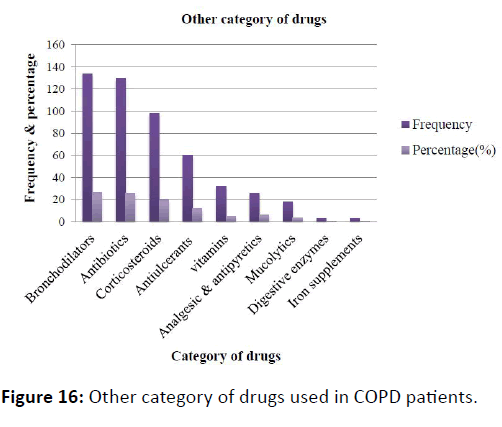
Other category of drugs used in COPD patients: Vitamins were commonly used and analgesics and antipyretic were also used to treat pyrexia and to overcome vitamin deficiency in COPD patients (Figure 16, Table 9).
| Category | Frequency | Percentage (%) |
|---|---|---|
| Vitamin supplements | 32 | 37.6 |
| Analgesic &antipyretic | 25 | 29.5 |
| Mucolytics | 22 | 25.9 |
| Digestive enzymes | 3 | 3.5 |
| Iron supplements | 3 | 3.5 |
Table 9: Other category of drugs used in COPD patients.
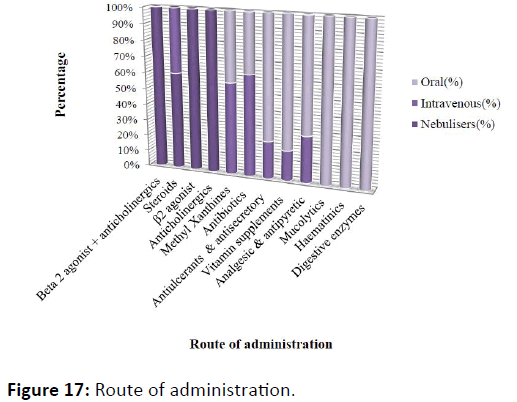
Route of administration: In the 60 patients mostly used route is nebulizers (β2 agonist + anticholinergics) to treat the exacerbation of the symptoms followed by the steroids which are used in both inhalation and the intravenous route (Figure 17, Table 10).
| Category | Nebulisers (%) | Intravenous (%) | Oral (%) |
|---|---|---|---|
| Beta2agonist + anticholinergics | 42.5 | - | - |
| Steroids | 38.6 | 25.5 | |
| β2 agonist | 10.6 | - | - |
| Anticholinergics | 8.3 | - | - |
| Methyl Xanthines | - | 14.5 | 10.8 |
| Antibiotics | 45.5 | 26.6 | |
| Antiulcerants&antisecretory | 6.8 | 22.3 | |
| Vitamin supplements | 3.4 | 14.6 | |
| Analgesic & antipyretic | 4.3 | 10.4 | |
| Mucolytics | 11.9 | ||
| Haematinics | 1.7 | ||
| Digestive enzymes | 1.7 |
Table 10: Route of administration.
Discussion
The study was conducted in 60 COPD patients among which 30 were control and other 30 were intervention group. Present study showed that COPD is more predominant in male population. The Patients in the age group of 61-80 years were mainly affected both in intervention i.e., (60%) and control group (56%). Similar report was found by Ramanath et al. [9] and less number of people was found in the age group of 21-40 i.e., (13.3%) in control group and (26%) in intervention group. Equal number of literates were found 15 (50%) in both control and test groups. There is high percentage of smokers in both intervention 28 (93.3%) and control 25 (83.3%) group. The main part of the study is medication adherence, it was found that there no significant difference at baseline, followed by first follow up was <0.01*, followed by second follow up was <0.0001***. This clearly showed that there was a good improvement in medication adherence behavior of COPD patients in intervention when compare to control because the intervention group patients were provided with effective counseling materials. It concluded that pharmacist intervention plays an important role in improving adherence. But there was slight improvement in control group this may be due to repeated visits to hospital. The patients are motivated to follow the medications regularly as prescribed but some may fail to some reasons so the pharmacist intervention is very important to improve the adherence to medications.
During the study it was observed that a total number of 461 drugs of different class were prescribed in the prescription of 60 COPD patients. An average of 7-8 drugs was prescribed in each prescription. In this bronchodilators are used as a combination therapy i.e., β2 agonist + anticholinergic (Salbutamol + ipratropium bromide) 56 (46%) most commonly used drugs in the COPD patients, followed by monotherapy, methyl xanthenes 41 (33.6%), β2 agonist 14 (11.4%) and anticholinergics 11 (9%).
Among the patients, 88 corticosteroids were prescribed in the prescription in which systemic corticosteroids were (42%) and inhaled corticosteroids (58%) were used more than the systemic corticosteroids. It is observed that in 60 patients different class of antibiotics were used among them cephalosporin antibiotics 29 (25.2%) were used in high number than other class of antibiotics like penicillin’s 23 (20%) and macrolides 22 (19.3%) most of this were given in IV route.
It was observed that out of 60 patient’s high percent 18 (35.2%) of H2 receptor antagonists (ranitidine) were used and the less percent of Proton pump inhibitors + antiemetic 9 (17.7%) (Rabeprazole + domperidone) were used as antiulcerants and other category of drugs used in COPD patients was found to be vitamins 32 (37.5%) were commonly used for general weakness and analgesics and antipyretic 25 (29.5%) were used to treat pyrexia and mucolytics 22 (25.9%).
Conclusion
A total of 60 patients were enrolled in this study. The 30 patients were considered as control group and other 30 were considered as intervention group. The adherence to the therapy was low in the test group at the base line and as the patients were counseled, the adherence to that medication was progressively increased for the first and second follow ups. In over all, high adherence to the therapy was seen in COPD patients in the intervention group compared to that of control group.
More number of smokers are suffering with the disease and patient education has achieved the optimal results in quitting the smoking and reduces exacerbation of symptoms and improved medication adherence.
The utilization of β2 agonist+anticholinergics, corticosteroids and methylxanthines were observed to be more commonly used to treat the exacerbations of the symptoms.
By providing effective counselling and there is improved medication adherence to treatment in the test group and the p value was found to be highly significant i.e., <0.0001***.
References
- Shargel L, Mutnick AH,Swanson LN, Souney PF (2013) Comphrehensive pharmacy review. Walter’s kluwer.pp: 852-860.
- Mohan H (2010) Textbook of pathology. Jaypee brothers.pp: 477-482.
- Tripathi KD (2010) Essentials of medical pharmacology.Jaypee brothers.pp: 217-225.
- Vestbo J, Hurd SS, Agusti AG, Jones PW, Vogelmeier C, et al. (2003) Global strategy for the diagnosis, management and prevention of COPD. Am J RespirCrit Care Med 187: 347-365.
- Wouters EF, Creutzberg EC, Schols AM (2003) Systemic effects in COPD. Chest 121: 127S-130S.
- Parthasarathi G, Nyfort-Hansan K, Nahata MC (2013) A textbook of clinical pharmacy practice: Essential concepts and skills Universities press.pp: 441-447.
- Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353:487-497.
- Mitchell DM(2001) Introduction to Chronic obstructive pulmonary disease. Thorax 56: 1-2.
- Ramanath KV, Nagakishore CH, Mahesh S, Balaji D, Bhanuprakash M (2011) A study on medication adherence and quality of life in asthma and COPD of rural population, in a tertiary care hospital. Indo Global J Pharm Sci 1: 315-327.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences